The leukogram or leukon includes all tests that evaluate WBC, including the following:
- Assessment of leukocyte numbers: Total WBC count (all cell types), relative (%) and absolute (cells/uL) differential leukocyte count (WBC separated by type).
- WBC morphologic features: These can give clues as to underlying disease pathogenesis or can identify the cause of the anemia, including parasites.
WBC count
The WBC count is the total number of leukocytes in a volume of blood, expressed as thousands/µL. As with the RBC, the WBC can be done by manual methods or by automated cell counters. The WBC by any method is a count of nuclei or total nucleated cell count. If nucleated red blood cells (nRBC) are circulating in blood, they will be included in the nucleated cell count whether the count is done by manual methods or by automated analyzers. In such cases, the WBC represents the leukocyte count only after it has been corrected for the nucleated red cells (nRBCs). The number of nRBCs per 100 leukocytes is recorded during the differential leukocyte count. Then a correction is made as follows:
Corrected WBC = nucleated cell count x (100 ÷ [nRBC + 100])
In reports from our laboratory (excluding automated hematology tests), the WBC value is usually a leukocyte count since we correct for the presence of nRBCs if > 5 nRBCs are counted in a 100 cell differential WBC count.
Differential WBC count
This is done by counting 100 leukocytes in the monolayer of the smear, which provides relative proportions (percentages) of WBC normally found in blood. This can be converted to an absolute count (thousands/uL) by multiplying the percentage by the total WBC count. The following leukocytes are counted in a 100 differential cell count: neutrophil (mature segmented forms), bands (immature neutrophils, band forms are the most common), lymphocytes, monocytes, eosinophils and basophils.At Cornell University, we also use the “Other WBC” category to include cells of hematopoietic origin that are not normally seen in blood, such as mast cells, histiocytes or blasts associated with a leukemia. More information is given about each of these categories below.
Neutrophils
Neutrophils are innate immune cells that are produced in bone marrow, released into blood after completing their maturation in marrow, circulate for less than a day (10-15 hours), and migrate out of the vessels into tissues or body cavities. While circulating, neutrophils are distributed between large vessels (neutrophils here form the circulating neutrophil pool or CNP) and small vessels (neutrophils here form the marginating neutrophil pool or MNP). The total body neutrophil pool (TNP) comprises the CNP, MNP, and the pool of post-mitotic neutrophils in marrow. Only the circulating neutrophil pool is sampled. Segmented neutrophils are considered fully mature cells and are the dominant leukocyte in the blood of dogs, cats, camelids and horses (and some ruminants).
Immature neutrophils
The presence of neutrophil lineage cells that are more immature than a segmented neutrophils in blood is generally called a left shift. The immature neutrophils are usually band neutrophils (horseshoe-shaped nuclei) but earlier stages, e.g. metamyelocytes, may be seen as well, depending on the severity of the tissue draw (inflammation) and marrow stores. Some laboratories quantify all immature stages separately, but this is not done at Cornell University, in which the band category (or count) includes more immature cells, such as metamyelocytes and myelocytes. This is because the left shift (immature neutrophils) is usually proportionate, i.e. more mature cells outnumber the more immature cells (bands > metamyelocytes > myelocytes). In the latter scenario, we usually flag the report to demonstrate the presence of cells of neutrophil lineage that are more immature than bands as this usually indicates a more severe tissue demand (inflammation) with release of less mature cells.
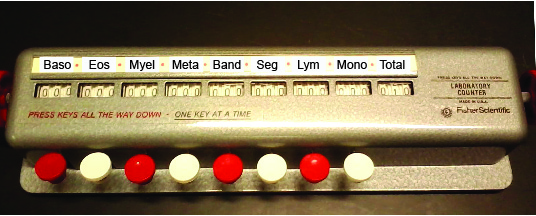
Neat historical fact: The origin of the word “left shift” is somewhat surprising. It is based on the use of old style cell counters, in which the manufacturers placed immature neutrophils to the left of mature neutrophils on the counter (www.pathologystudent.com) as depicted in the image below. With the advent of computers, the immature neutrophil button can be assigned to any key, however the term is here to stay and is used to indicate that there is the presence of more immature cells of a specific lineage in the circulation. The term is usually applied to neutrophils in blood.
Lymphocytes
Lymphocytes, unlike other leukocytes, are produced in lymphoid tissue rather than in bone marrow. Most lymphocytes in blood are long-lived cells that recirculate between blood and tissue. Changes in blood lymphocyte number usually reflect changes in distribution rather than changes in production or loss. Lymphocytes can be B cells (produce immunoglobulins), T cells (helper or cytotoxic) or natural killer cells. In normal canine, feline and equine blood, T cells dominate over B cells (roughly 3-4:1 ratio T:B). Lymphocytes are the dominant cell type in rodent blood and also in some cattle.
Monocytes
These large innate immune cells are produced in bone marrow, circulate briefly in blood, and migrate into tissues where they differentiate further to become dendritic cells or macrophages. There is no storage pool of monocytes in marrow; their numbers in marrow at a given time are very small. Monocytes in blood are unevenly distributed between a marginated and circulating pool.
Eosinophils
Eosinophils are produced in bone marrow, circulate in blood for a few hours, and migrate into tissues where they survive for several days. Increased production of eosinophils is mediated by factors produced by some activated T lymphocytes and mast cells, specifically interleukin-5. These are involved in allergic responses and immunity against parasites.
Basophils
Basophils are produced in bone marrow. Normally, the number in blood is very small in all species, but a few can usually be found in smears from healthy horses and ruminants. They are thought to be involved in immunity against parasites, like eosinophils.
“Other WBC”
We reserve this category if abnormal cells that are not normally seen in blood, are seen in sufficient numbers to be counted during a differential count (low numbers of these cells are just “flagged” in our assessment of WBC morphology). These include blasts (leukemia), histiocytes or macrophages (cells that resemble tissue macrophages and are demonstrating phagocytic activity in blood), and mast cells. These are only seen in diseased states.
Note, nRBC are counted during a differential count, but are not included as WBC. Rather, they have their own separate category. As indicated above, nRBC will alter (falsely increase) the total WBC count and their presence must be accounted for.
WBC morphology
We look for and semi-quantify the following changes, which help with interpretation of leukogram results:
- Toxic change (immature features): Cytoplasmic basophilia, Döhle bodies, cytoplasmic vacuolation, toxic granulation, immature chromatin. Semi-quantified as mild, moderate or marked. This usually indicates a tissue draw or demand (i.e. inflammation) and is a feature of accelerated maturation (giving the neutrophils insufficient time to mature properly before they are released, so they retain ribosomes and rough endoplasmic reticulum which can be seen as Dohle bodies or cytoplasmic basophilia) and release.
- Reactive lymphocytes (indicating antigenic stimulation): Semi-quantified as few, moderate or many.
- Smudged cells: These let you know how accurate the differential leukocyte count in. A few smudged cells will not impact the count but moderate to many will. Smudged cells are more frequently seen in “aged” or stored samples. Semi-quantified as few, moderate or many.
- Abnormal “other” cells: Presence of leukemic blasts, dysplastic changes in leukocytes, iron in leukocytes (sideroleukocytes), histiocytes, mast cells.
- Infectious agents: e.g. Anaplasma. Semi-quantified as few, moderate or many.
Leukogram patterns
Physiologic and pathologic processes cause certain alterations in the total and absolute differential WBC counts that can be recognized. Identification of these leukogram patterns is key to interpretation of changes in WBC in hemogram results. The usual patterns that we recognize from a hemogram are the following:
Physiologic leukocytosis
Due to epinephrine (fight-or-flight response). Characterized by a neutrophilia with no immature forms (no left shift) and lymphocytosis. An eosinophilia and basophilia may be seen in cats, in particular. Usually in young animals.
Stress leukogram
Due to endogenous corticosteroid release. Characterized by a neutrophilia with no left shift and a lymphopenia and eosinopenia. In some species, a monocytosis may be present (e.g. dogs).
Inflammatory leukogram
Due to inflammatory cytokines (interleukin-1, interleukin-6, tumor necrosis factor-α). Characterized by a left shift (regardless of total leukocyte numbers) or the presence of immature neutrophils in blood (band neutrophils typically; even earlier forms may be seen with severe inflammation). Toxic change is frequently seen as part of an inflammatory leukogram (but is not always present). Inflammation may result in a concurrent lymphopenia and eosinopenia, although this also could be due to a concurrent stress leukogram.
Leukemia
Leukemia is defined as the presence of neoplastic cells of hematopoietic origin in blood and/or bone marrow.
