Platelet counts can be done manually using a hemocytometer or with an automated analyzer. Counts can also be estimated during blood smear examination. Since many laboratories use instruments that count platelets, red cells and leukocytes concurrently, a platelet count is a routinely reported result on complete or automated hemograms. At the Clinical Pathology Laboratory of the Animal Health Diagnostic Center at Cornell University, we use the ADVIA hematology analyzer for obtaining platelet counts and verify the obtained count by estimating counts on a Wright’s-stained blood smear. Platelet counts are an essential component of the hemogram and are crucial for working up a bleeding patient. For more information on this diagnostic evaluation of a patient with a suspect hemostatic disorder, causes of thrombocytopenia (only listed in brief below) and additional information on performing platelet counts as part of hemostasis versus hemogram testing, refer to the hemostasis section of this website.
Methods
Automated platelet counts on the ADVIA
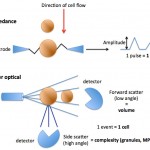
The ADVIA measures platelets by flow cytometry based on principles of light scattering. Platelets are identified by their size (< 30 FL, low angle light scatter) and refractive index (n = 1.35 to n = 1.40 or high angle light scatter).
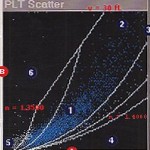
The platelet cytogram on the left is a graphical representation of how the ADVIA counts platelets. Low light scatter (refractive index or internal complexity) is plotted against the X axis and high light scatter (cell size) is plotted against the Y axis (B). Platelets are detected in the region labeled 1. Large platelets (section 2) are identified on the basis of size (> 20 FL) and refractive index (which distinguishes them from red blood cells, for the most part). In camelids with iron deficiency anemia or hemolyzed samples from any animal, small or lysed red blood cells may be erroneously counted as platelets, falsely increasing the platelet count.
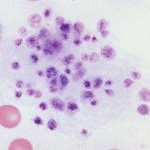
All blood smears are also examined for the presence of platelet clumps (see image to the right), which will affect the accuracy of the platelet count. Platelet clumps decrease the platelet count obtained by any method. Thus any provided count should be considered a minimum platelet count in the sample. In some samples with severe platelet clumps (many blood samples from cats), the platelet count is totally invalid. Under these circumstances (or any other situations resulting in erroneous counts, such as an iron deficient camelid), a platelet count will not be provided and the smear estimate of platelet numbers (increased, adequate, low? or low) given with our hemograms should be used as a guide as to the actual platelet count (see below).
Cats are notorious for platelet clumping (their platelets are activated at the slightest provocation) and it is difficult to obtain accurate counts in this species. Platelet clumping is usually due to a sample collection problem and can be minimized by collecting blood from a large peripheral vein (cephalic or jugular), such that blood flows smoothly into the vacutainer or syringe, and using a 22 or 23 G needle (in a dog or cat). The blood should be mixed with the anticoagulant as soon as possible after collection, by gentle rotation or inversion. Platelet clumping increases with time, so platelet counts should be done as soon as possible after collection to maintain accuracy.

Manual platelet counts
Platelet counts can be done manually with a commercial diluting system, hemocytometer, and a microscope. These counts are less accurate than automated counts, because platelets can be difficult to distinguish from debris. Platelet clumping will also decrease the hemocytometer platelet count.
Platelet count estimates from a blood smear examination
In a well-prepared smear, platelets are estimated by counting the average number of platelets seen per 100x oil immersion field in the monolayer. In general, 10 oil immersion fields are counted and the results averaged (this accounts for uneven dispersal of platelets in the smear). Then the following formula is applied (this is a rough guide):
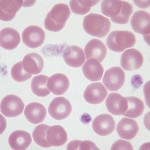
Estimated platelet count/µL = average count in 10 fields x 15,000
For example, if an average field contains 7 platelets, an estimate of 105,000/µL would be appropriate. This value would then be compared to the normal range for the species in question; 105,000/µL would be “low” (below reference intervals) for a dog, but “adequate” (or within reference intervals) for a horse.
At Cornell University, we provide a semi-quantitative estimate of platelet numbers which are based on reference intervals for the species in question (if available) as follows:
- Increased (Incr.): The count is above the reference interval for the species.
- Adequate (Adeq.): The count is within the reference interval for the species.
- Low?: The count is within the low end of the reference interval for the species or may be mildly decreased (i.e. the count is “equicovally low”).
- Low: The count is below the reference interval for the species.
- Very low: The platelet count is below a medical decision limit associated with spontaneous hemorrhage, i.e. <30,000/uL.
Test interpretation
Decreased platelet number (thrombocytopenia)
Causes of thrombocytopenia fall into one or a combination of the following general mechanisms:
- Artifact of collection (e.g. clumping)
- Iatrogenic: Hemodilution
- Decreased production of platelets in the marrow
- Increased consumption of platelets in coagulation
- Increased destruction/clearance of platelets by macrophages
- Sequestration of platelets in the spleen or microvasculature
- Loss with acute severe hemorrhage
Please refer to the hemostasis section of the website for more information on platelet counts (including a brief mention of critical values) and disorders causing thrombocytopenia (including a table on bleeding risk at different platelet counts).
Increased platelet number (thrombocytosis)
Thrombocytosis may occur in primary myeloproliferative conditions or as a secondary (reactive) phenomenon in a variety of physiologic and pathologic states. Thrombocytosis is usually due to an increase in platelet production and release (in reactive cases, this is likely due to increased thrombopoietin or other thrombogenic cytokines, such as interleukin-6), rather than an increased platelet lifespan. Usually, a platelet count higher than the reference interval for the species is a reactive thrombocytosis, and not of direct pathologic importance. Young animals, in particular calves and foals, normally have platelet counts higher than the adult reference interval.
Further discussion on thrombocytopenia and thrombocytosis is found under disorders of platelet number.
